When allergy season rolls around, over 50 million people around the country experience uncomfortable symptoms that affect their everyday lives. With COVID-19 continuing to present a concern, especially for people with underlying health conditions, it’s important to be able to quickly distinguish between allergy and COVID-19 symptoms. Having an experienced allergist you can turn to is essential in getting help for your symptoms while making sure you’re not suffering from COVID-19.
Doctors now know that treating COVID-19 early is important in limiting severe outcomes. Therefore, knowing how to differentiate between the two ailments and seeking appropriate help will ensure you achieve a speedy recovery and remain comfortable, regardless of whether you’re dealing with allergies or the coronavirus.
What Are Allergies?
Allergies are the response your immune systems mounts against a substance it sees as an invader. These triggering substances or stimuli are called allergens and can range from dust and pollen to mold, pollution and chemicals.
Not all people with allergies react to the same stimuli. Furthermore, the severity of the reaction can span from an annoying skin condition to a life-threatening response.
COVID-19 Symptoms
COVID-19 is the illness that the SARS-CoV-2 virus causes when it manages to affect the immune system. Many people can become infected with the virus but continue to carry it asymptomatically. This means that the virus does not progress to COVID-19.
Asymptomatic carriers vary from presymptomatic infections. Presymptomatic refers to people that have the virus in their system but will exhibit symptoms over the coming days. If you have a strong immune system or were exposed to a small SARS-CoV-2 viral load, you may remain without symptoms.
Let’s look at what COVID-19 symptoms look like, from the early stages of the illness up to the need for hospitalization. The most common symptoms reported include cough, fever, chills, runny nose, congestion and difficulty breathing.
From the early manifestation of COVID-19 in your body, you may experience fatigue and sore throat. Though it can occur at any time, many patients will find that around the five to seven-day mark, they will experience a loss of taste, smell or both.
COVID-19 sufferers may also experience nausea and vomiting which can be exacerbated by an intense cough.
Allergy Symptoms
Allergies can result in several symptoms that keep you from enjoying your daily schedule. When your immune system detects an allergen, either through skin contact, breathing or ingestion, a number of inflammatory symptoms will start to appear.
Pollen or other environmental allergies can cause sneezing, runny nose, watery eyes, itchy sinuses, and sore throat. Symptoms also include itchy sinuses, itchy throat, ear congestion, skin rash, postnasal drainage and headache. As a result of your immune system reacting to allergens, you may also feel fatigued and have shortness of breath.
Sinus infections can cause similar symptoms, causing you to mistake them for an allergic reaction. A sinus infection may result in difficulty sleeping whereas many allergies may subside as you prepare for bed. In any case, a doctor can conduct a differential diagnosis to confirm or eliminate an infection.
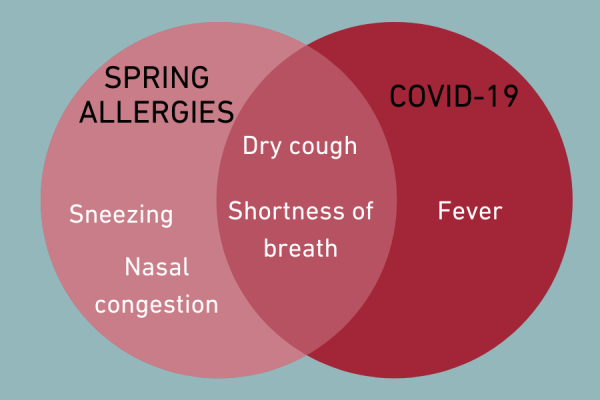
Similarities Between COVID-19 and Allergy Symptoms
Understanding the similarities between COVID-19 and allergies will help you take early action so that you can deal with the respective cause. Both of these conditions can cause runny nose, cough, sore throat, shortness of breath, fatigue and nasal congestion. Your allergy doctor can advise you on what you need to do to arrive at the root cause of your symptoms.
Seasonal allergies will not cause fever, chills, loss of taste and smell, nausea, vomiting or diarrhea. If you find yourself with any of these symptoms, it doesn’t necessarily mean you have COVID-19. It does mean, however, that you should contact your doctor about determining what the underlying cause of your illness is.
COVID-19 Prevention
To avoid COVID-19, keeping your distance from people that appear to be sick is a basic, prudent measure. Limiting your exposure to carriers of the virus can be achieved by steering clear of crowded spaces. Transmission is far less likely in outdoor spaces where you can keep at least six feet between you and others.
Boosting your immune system with vitamin D, vitamin C and other supplements can be done upon getting your doctor’s recommendations. Exercising and improving your mental state will only contribute to a more effective immune system that can deal with intruders efficiently.
Furthermore, the CDC suggests masks in indoor spaces and COVID-19 vaccines which have beem made available.
Dealing With Allergies
Allergies can limit your ability to function at school, in the workplace or socially. Your productivity suffers and your capacity to enjoy social activities goes out the window.
More importantly, keeping your allergies in check can ensure you stay out of harm’s way. Anaphylactic shock and allergy-triggered asthma attacks can potentially be life-threatening. Luckily, there are things your allergy doctor can suggest to bypass the uncomfortable symptoms, keep you safe and allow you to pursue your daily schedule.
Medication
Antihistamines are the most commonly prescribed medication for allergies. They can come in the form of nasal sprays, eye drops, pills or liquids. Antihistamines, as the name suggests, combat the histamines that irritate your immune system.
Histamines are one of your immune system’s greatest allies. When an irritant enters your body, these chemicals spring into action to protect you.
In the case of allergies, pollen and other irritants are otherwise harmless substances. Being allergic means that your immune system overreacts, causing inflammation through the production of histamines. Anti-histamines keep this process in check.
If your allergy-induced inflammation needs something more potent than anti-histamines, your doctor may give you corticosteroids.
Besides countering inflammation, your doctor may prescribe decongestants for freeing up your sinuses. You can obtain certain decongestants over the counter if you need to clear your sinuses. Keep in mind that those suffering from cardiovascular disease, high blood pressure, hyperthyroidism and glaucoma should avoid decongestants.
Allergy Immunotherapy
Immunotherapy is the process by which your doctor trains your immune system to react to an ailment more favorably. With allergy immunotherapy, your allergy doctor introduces small doses of an irritant into your body. This causes your immune response to be more tempered upon encountering the allergen in the future.
While immunotherapy doesn’t resolve allergies overnight, it provides a sustainable and more comfortable way of dealing with symptoms. Although allergies are never cured, so to speak, your body will learn to not overreact to substances that previously causes you to throw away weeks of your life because of pesky symptoms.
In effect, your body will reach a point where an occasional maintenance treatment will be enough to keep severe symptoms at bay. A consultation with an allergy doctor will give you a better idea of what you can expect from immunotherapy.
Which Allergy Treatment Is Best for You?
If you’re experiencing flu-like symptoms, look through the symptoms mentioned above to try and pinpoint whether you need COVID-19 treatment or a consultation with your allergy doctor instead.
Alleviating allergy symptoms can keep you from wasting weeks or even months of your productivity each year. Upon arriving at an allergy diagnosis, ask your doctor which treatment option is best for you. Make your well-being a top priority and always take a proactive approach to your health!